Preventive Dentistry

What is a Tooth Abscess?
A tooth abscess is a pocket of pus caused by a bacterial infection. It can occur in different parts of the tooth including the tip of the tooth root, the side of the tooth root, and the gums. Each different type of tooth abscess has its unique name:
- Periapical Abscess: Found at the tip of the root.
- Periodontal Abscess: Found in the gums at the side of a tooth root.
- Gingival Abscess: Found in the gums.
Symptoms of a Tooth Abscess
Recognizing the symptoms of a tooth abscess is crucial for getting timely treatment. Common symptoms include:
- Painful, persistent toothache that may spread to your jaw, neck, or ear.
- Tooth sensitivity to hot and cold.
- Swelling in your face or cheek.
- Tender, swollen lymph nodes, particularly in the neck or under the jaw.
- Foul taste in your mouth or chronic bad breath.
- Difficulty swallowing or breathing.
A tooth abscess is a serious condition that requires prompt dental attention. If you experience any of these symptoms, contact our dental office in Sparks immediately for an evaluation.
Causes of a Tooth Abscess
Several factors can lead to a tooth abscess. Common causes include:
- Poor dental hygiene
- High sugar diet
- Tooth decay
- Gum disease
- Dental injury
Preventing a Tooth Abscess
Understanding the causes of a tooth abscess can also help you take preventive measures. Some ways you can help protect yourself against a tooth abscess are:
- Brushing twice a day and flossing daily.
- Reducing sugar intake.
- Treating dental issues promptly.
- We visit our dental office in Sparks every six months for check-ups.
Treatment Options for a Tooth Abscess
If you have a tooth abscess, there are several treatment options available.
- Draining the abscess to remove the infection.
- Root canal therapy to clean out the infected pulp inside the tooth.
- Antibiotics to help eliminate the infection.
- Tooth extraction in severe cases.
If you’re experiencing any symptoms of a tooth abscess or need regular dental care, don’t wait. Contact our dental office in Sparks today. We are committed to providing comprehensive dental services to keep your smile healthy and pain-free. Our experienced team is here to help.
You’ll always hear your dentist in Sparks say just how important brushing and flossing are to your oral and overall health. However, the order in which these tasks are performed can significantly impact their effectiveness. Let’s explore the proper steps to take when flossing and brushing your teeth, emphasizing the crucial role of flossing before brushing.
Step 1: Begin with Flossing
Flossing is often an overlooked but vital step in achieving optimal oral health. It helps remove plaque and food particles from between your teeth and along the gumline, areas that a toothbrush alone may struggle to reach. Flossing before you brush your teeth will help loosen up any of these lingering pieces of food, bacteria, or plaque and then you can brush them away. To ensure you get the most out of your flossing routine, follow these steps:
- Choose the Right Floss: There are various types of dental floss available, including waxed and unwaxed, flavored and unflavored, and dental tape. Select one that suits your preference to encourage consistent use.
- Take an Adequate Amount of Floss: A general rule of thumb is to use about 18 inches of dental floss. Wind most of it around the finger of one hand and the rest around another finger of the other hand, leaving a few inches of floss in between.
- Use Proper Technique: Hold the floss between your thumbs and index fingers, leaving a one-inch section for cleaning. Gently slide the floss between your teeth, curving it around each tooth in a ‘C’ shape. Be careful not to snap or force the floss as it may injure your gums.
- Clean Both Sides of Each Tooth: As you move from tooth to tooth, ensure you clean both sides of each tooth, reaching down to the gumline. This comprehensive approach helps eliminate hidden plaque and bacteria.
Step 2: Move on to Brushing
Now that you’ve thoroughly cleaned the spaces between your teeth, it’s time to move on to brushing. Brushing helps remove remaining plaque, bacteria, and debris from the surfaces of your teeth. Here’s how to make the most of your brushing routine:
- Choose the Right Toothbrush: Select a toothbrush with soft bristles to avoid damaging your enamel and gums. Electric toothbrushes can also be effective, providing consistent and thorough cleaning.
- Apply the Right Amount of Toothpaste: A pea-sized amount of fluoride toothpaste is sufficient for effective cleaning. Excessive toothpaste can lead to foaming and may not provide additional benefits.
- Brush in Circular Motions: Hold your toothbrush at a 45-degree angle to your gums and brush in gentle circular motions. Ensure you cover all surfaces of your teeth, including the fronts, backs, and chewing surfaces.
- Don’t Forget Your Tongue and Gumline: Gently brush your tongue to remove bacteria and refresh your breath. Additionally, pay attention to your gumline, as this area is prone to plaque buildup.
- Replace Your Toothbrush Regularly: If your toothbrush bristles become frayed or worn, it’s time for a replacement. Old toothbrushes may not clean your teeth effectively and can harbor bacteria.
By following this comprehensive flossing and brushing routine, you can significantly enhance and protect your oral health. Remember, consistency is key. Aim to floss and brush at least twice a day, and don’t forget to schedule regular dental check-ups and cleanings with your dentist in Sparks.

Understanding the Need for a Root Canal
A root canal becomes necessary when the innermost layer of a tooth, the pulp, becomes infected or inflamed. This can occur due to deep cavities, repeated dental procedures on the same tooth, or traumatic injuries. The pulp contains nerves, blood vessels, and connective tissue, and when it becomes infected, it can cause severe pain and lead to the formation of abscesses if left untreated.
Debunking Root Canal Pain Myth
The fear associated with root canals is largely rooted in the misconception that the procedure itself is excruciatingly painful. However, advancements in dental technology and anesthesia have transformed the root canal experience. In reality, the purpose of a root canal is to alleviate pain, not cause it. The procedure itself is now quite straightforward.
- During a root canal, your dentist will remove the infected or damaged pulp
- Then, they’ll clean and disinfect the tooth’s interior
- Finally, the tooth is sealed to prevent further infection.
Modern techniques and advancements are used to numb the tooth and surrounding area, ensuring you feel little to no pain during the procedure.
Modern Techniques
- Anesthesia
One of the primary reasons for the historical fear of root canals is outdated anesthesia techniques. In the past, numbing the affected area might not have been as effective, leading to discomfort during the procedure. However, contemporary dentistry uses highly advanced and targeted anesthesia methods, ensuring patients are comfortable and pain-free throughout the process.
- Technology and Equipment
Advancements in dental technology have also played a crucial role in making root canals more efficient and less intimidating. High-tech equipment, such as rotary instruments and magnification devices, allows your dentist in Sparks to perform the procedure with greater precision. This not only reduces the time required for the root canal but also minimizes the chances of complications.
What to Do After a Root Canal
Once the root canal is complete, patients often experience relief from the pain and discomfort caused by the infected pulp. In some cases, mild soreness or discomfort may be present for a short period. But following the recommendations of your dentist in Sparks, which often includes over-the-counter pain relievers, is usually sufficient in managing any post-procedure discomfort.
The Importance of Root Canals
While nobody wants to hear that they need a root canal, the truth is a root canal should be viewed as a valuable procedure that can save a tooth from extraction. Losing a natural tooth can lead to a range of issues, including difficulty chewing, changes in bite alignment, and a higher risk of other dental problems. Root canals help preserve the natural structure of the tooth, maintaining oral health and function.
The fear surrounding root canals is largely unfounded in the modern era of dentistry. Understanding the reasons why someone might need a root canal and dispelling the myth of unbearable pain can empower individuals to make informed decisions about their dental health. With advanced anesthesia techniques, state-of-the-art technology, and skilled dental professionals, a root canal is not something to fear but rather a crucial step toward preserving your natural smile.
If faced with the possibility of a root canal, approach the procedure with confidence, knowing that it is a routine and pain-relieving dental intervention.
We’ve all caught ourselves biting our cheeks from time to time, which is a seemingly harmless habit that can often be attributed to stress, anxiety, or even just absentmindedness. While it might not seem like a big deal at first, your dentist in Sparks knows that consistently biting your cheeks could potentially lead to problems for your teeth and overall oral health. But why exactly is this habit problematic and what can you do to decrease the dental risks associated with it?
The Habitual Cheek Bite
Biting your cheeks might seem innocuous, but when done regularly, it can have repercussions beyond just temporary discomfort. Habitual cheek biting involves repeatedly clenching your teeth down on the soft tissue of your inner cheeks. Over time, this can cause irritation, inflammation, and even result in sores or ulcers in the mouth. While these symptoms might be uncomfortable on their own, they can also indirectly affect your teeth.
Dental Damage: Consistent cheek biting can create pressure on your teeth. This constant pressure can result in micro-fractures, chips, or cracks in your teeth. Over time, this damage might necessitate dental treatments such as dental bonding, fillings, or even crowns to restore the affected teeth.
Shift in Tooth Alignment: Habitual cheek biting can also affect the alignment of your teeth. The repetitive movement of your teeth against the cheek can push them out of their natural positions, potentially leading to malocclusion or misalignment. This might require treatment from your dentist in Sparks to correct the issue.
Bruxism Aggravation: Cheek biting is often associated with bruxism – the habit of clenching or grinding your teeth, usually during sleep. Bruxism can lead to enamel erosion, tooth sensitivity, and jaw pain. Habitual cheek biting can exacerbate these issues, intensifying the impact of bruxism on your dental health.
Prevention and Management
There are several ways you can prevent dental damage caused by habitual cheek biting including:
Awareness and Mindfulness: The first step in addressing cheek biting is to become more aware of when you’re doing it. Pay attention to moments when you catch yourself biting your cheeks, and try to identify any triggers. Practicing mindfulness and stress reduction techniques can also help minimize the instances of cheek biting.
Mouthguards: For those who find it challenging to control cheek biting, your dentist in Sparks can create custom mouthguards or splints to help. These devices act as a barrier between your teeth and cheeks, preventing direct contact and reducing the potential damage caused by clenching and grinding.
Biting your cheeks might seem like a minor concern, but its impact on your dental health can be significant. From dental damage and misalignment to exacerbating bruxism-related problems, this seemingly harmless habit can lead to various oral health issues. The key lies in awareness, stress management, and seeking professional guidance when needed. By taking steps to address and mitigate cheek biting, you can preserve your dental health and maintain a confident smile for years to come. Remember, a proactive approach to oral health can lead to a happier and healthier mouth.
Even though dentists are primarily associated with oral health, there’s a lesser-known aspect of dentistry – its role in treating migraines and headaches. Some dentists’ expertise can extend beyond the realm of teeth and gums and into other systemic health concerns such as the connection between migraines, headaches, and dental health In fact, your dentist in Sparks may be able to provide much-needed relief to those suffering from chronic headaches.
The Dental-Migraine Connection
Migraines and headaches affect millions worldwide, impacting individuals physically, emotionally, and socially. But what many don’t realize is that dental issues, such as temporomandibular joint disorder (TMJ), misaligned bites, and teeth grinding (bruxism), can contribute significantly to the frequency and intensity of these debilitating headaches.
TMJ Disorder
Temporomandibular joint disorder, a condition affecting the joint that connects the jawbone to the skull, often goes undiagnosed but can certainly cause symptoms including headaches and migraines. Dentists are trained to identify the telltale signs of TMJ disorders, such as jaw pain, clicking noises, and limited jaw movement. Addressing TMJ issues can lead to remarkable improvements in migraine and headache symptoms.
Malocclusion
A malocclusion, commonly known as a “bad bite,” occurs when the upper and lower teeth do not align correctly. This misalignment can lead to increased muscle tension, which triggers headaches. Dentists can conduct bite assessments and orthodontic treatments to rectify malocclusions, potentially offering relief to headache sufferers.
Bruxism
Bruxism, the unconscious clenching, and grinding of teeth, is a common dental issue often linked to stress and anxiety. Prolonged bruxism can strain the jaw muscles, leading to headaches.
Dental Solutions for Headache Relief
Depending on the underlying cause of headaches or migraines, your dentist in Sparks may be able to help you get relief.
- Mouthguards
Dentists can create custom mouthguards or suggest stress management techniques to alleviate bruxism and its related headaches.
- Orthodontics
Orthodontic treatments, such as braces or clear aligners, can correct malocclusion, which in turn can reduce the frequency and intensity of headaches. Through carefully planned orthodontic procedures, dentists can achieve a harmonious bite, promoting overall oral health and reducing headache triggers.
- TMJ Therapies
Dentists equipped with TMJ disorder treatment knowledge can offer targeted therapies and techniques like ultrasound therapy, trigger point injections, and jaw exercises to provide immense relief to migraine sufferers.
Nobody should have to deal with chronic headaches or migraines. Dentists can help. Those who have tried other treatments but have not yet considered a migraine-dental connection are encouraged to consult their dentist in Sparks for an evaluation. They just may unlock the relief you’ve been seeking for a happier, pain-free life.

What Is a Cavity?
Cavities are so common in the United States that the CDC says 90% of Americans over the age of 20 have had at least one cavity in their lifetime. These tiny areas of tooth decay, if left untreated, will only become bigger and deeper and also become more difficult to treat. Cavities begin as a small hole or pit in a tooth where acid or bacteria has attacked the enamel. During this stage, cavities can easily be fixed with a filling from your dentist in Sparks. However, cavities that continue to progress can sometimes require more complex treatment such as a root canal or even tooth extraction.
Surprising Things The Cause Cavities
We’ve already shared that many people think cavities are a problem of eating too much sugar, and while that may be the case, there are other reasons why a cavity develops.
- Dry Mouth
If a patient’s mouth is dry it’s more likely that they will have cavities. Usually, saliva will help neutralize acids and rinse away bacteria that can cause cavities. But when saliva production is too low and the mouth feels too dry, bacteria and acids are left lingering around to cause damage to the enamel and, you guessed it, cause cavities.
- Carbohydrates & Acids
Besides sugar, there are other foods that can increase the risk of cavities. The two most concerning are acidic foods, such as citrus fruits and foods with a lot of carbohydrates. Acidic foods and drinks further aid in the mouth acid’s ability to weaken enamel while carbs fuel the bacteria, allowing them to thrive.
- Bad Brushing or Flossing
There are many reasons why it’s important to brush your teeth twice a day and floss once a day, but one of the main reasons is to prevent cavities. Brushing your teeth in the morning and at night will remove plaque and plaque acids that have built up throughout the day. Flossing reaches those tricky areas that a toothbrush can’t reach and where cavities are more likely to develop.
Cavity Symptoms
Patients may experience different symptoms, but some of the most common signs of a cavity include:
- Pain when you bite
- Tooth sensitivity
- Brown, black, or white spots
- Toothache
- Pits or holes in a tooth
If you think that you may have a cavity, call your dentist in Sparks to schedule an appointment.
Even though cavities are incredibly common, there are things you can do to reduce your risk of getting one. Make sure you brush and floss your teeth regularly, limit your intake of sugary, acidic, or high-carbohydrate foods, and drink plenty of water daily. Of course, you should also see your dentist every six months for a checkup.

Let’s Talk Tooth Sensitivity
Have you ever had a cold or hot beverage that made your teeth feel funny? This is something we call tooth sensitivity, and it’s actually a normal side effect after you’ve completed dental work like cavity fillings, tooth extractions, or dental implants. Why does tooth sensitivity lead to dental pain? It’s due to nerve inflammation inside your tooth or teeth. If you have pain or tooth sensitivity that persists for weeks or even months after you’ve seen your Sparks dentist, you’ll want to schedule an appointment to have them take a look at your teeth to see if something needs further attention.
It’s All About Pressure
When unwanted discomfort occurs after a filling or any dental treatment, you’re probably wondering why. It turns out the answer to this question is simple — it’s pressure. After your filling is permanently in place, the piece of your tooth that was damaged by bacteria is now filled in, adding new pressure to the area. This can change how air and saliva move across your tooth, causing sensitivity.
What You Can Do to Feel Better
You can take some steps at home to help you feel better if you have dental discomfort or pain post-procedure. Try taking some Advil, Ibuprofen, or Aleve. Be sure to follow the recommended dosage directions and instructions. Applying a cold compress on your cheek or jaw to minimize pain. Are you also wondering how to manage sensitivity in your teeth due to cracks and damages to a filling? Maintaining optimal dental health should still be your top priority, and you want to:
- Use a toothpaste specially designed for sensitive teeth
- Brush and floss regularly every day
- Gargle using warm, salty water
The right thing to do if you’re experiencing any pain, discomfort, or sensitivity is to schedule a visit right away at our Sparks dental office. We can help you feel better and determine what’s causing your issues so we can get to the root of the pain. If you have any questions or concerns, please feel free to call our office today and chat with us. We’re always here to help and look forward to hearing from you!
Each and every February, loved ones throughout the United States go above and beyond preparing for Valentine’s Day. Whether you choose to show your love with chocolates or flowers, one thing remains constant — bright red hearts are everywhere we look. But there’s another reason (besides Valentine’s Day) that we should pay attention to these hearts. February is American Heart Health Month and focuses on raising awareness of how daily choices affect our risk of heart disease. In fact, this holiday has a special place in your Sparks dentist’s heart because there is a strong connection between oral health and heart health.
What is Gum Disease?
Gum disease is an infection in the gum tissues usually caused by a buildup of bacteria and plaque. When someone doesn’t brush their teeth often enough or well enough, plaque is left behind and can easily work its way up under the gum, settle in, and cause trouble.
There are four stages of gum disease including:
- Gingivitis
- Slight Periodontal Disease
- Moderate Periodontal Disease
- Advanced Periodontal Disease
Gum disease can be treated if caught in the gingivitis stage, so make sure you visit your dentist in Sparks every six months for dental cleanings, x-rays, and thorough exams so we can identify any problems early.
What Does This Have to Do With Your Heart?
If gingivitis isn’t diagnosed and treated quickly it will progress into slight, moderate, or advanced periodontal disease, all of which are irreversible. When gum disease progresses into these advanced stages, the infection can enter the bloodstream and travel throughout the body. This can affect areas outside of the mouth, including the heart.
Heart Disease
Bacteria from gum disease in the bloodstream causes the body to produce too much C-reactive protein (CRP). Higher than normal levels of CRP can lead to serious conditions such as:
- Inflamed arteries
- Blood clots
- Heart attacks
- Strokes
Knowing that your oral health can have such an impact on your overall wellness makes it so incredibly important that you practice good oral hygiene habits at home, including brushing twice a day for two minutes and flossing every day.
Signs of Gum Disease
Since early diagnosis is so crucial to treating gum disease before it has the chance to affect the rest of your body, you need to know the signs of gum disease. Keep an eye out for:
- Bleeding when brushing or flossing
- Puffy, tender gums
- Bad breath
- Loose teeth
If you notice any of the signs of gum disease, call your dentist in Sparks to schedule an appointment. This American Heart Health Month, commit to reducing your chances of heart disease by brushing and flossing every day, seeing your dentist in Sparks twice a year, exercise, and eat a healthy diet. For more ideas on how to live a heart-healthy life, visit the National Heart, Lung, and Blood Institute.

What is Plaque?
When trying to remember the difference between plaque and tartar, it may help to think of the two Ps. Plaque is the primary, or first, thing that can affect your teeth. Plaque is a sticky film that’s basically made up of millions and millions of bacteria. It naturally builds up on teeth throughout each day, and as we eat, the plaque bacteria are also eating. As a byproduct of this feeding, the bacteria release acids. These acids can erode tooth enamel, weaken teeth, and make it easier for cavities to form. However, when we effectively remove plaque through brushing, we can help reduce the number of bacteria and lower the risk of decay and the need for fillings from your Sparks dentist.
What is Tartar?
So what happens when plaque remains on the teeth for too long? That’s where tartar comes into play. When plaque isn’t effectively removed it will harden into tartar. Now, while plaque can be cleaned away through at-home brushing, tartar is a different story. Once plaque hardens into tartar it can’t be removed through regular brushing. Your dentist in Sparks will need to intervene to thoroughly remove tartar buildup. If tartar is not removed, it can increase the risk of cavities, cause tooth discoloration or tooth sensitivity, and can even lead to gum disease.
How to Avoid Plaque and Tartar Buildup
Avoiding plaque buildup and, in turn, tartar isn’t difficult, but it does require good oral hygiene habits. Make sure you’re brushing your teeth each morning and before bed every night for two minutes each time. Additionally, it’s important to remove plaque that may have accumulated in between teeth by flossing once a day. In between brushings, try to drink plenty of water to help neutralize and rinse away acids, and also to remove bacteria. You can also chew sugarless gum after meals and snacks. And as always, try to avoid sugary sweets and drink as it will make for both a happier, healthier smile and a happier dentist.
The truth is, everyone’s teeth will accumulate some plaque and some tartar. The important thing to remember is that this buildup needs to be removed through both brushing and flossing properly at home and seeing your dentist regularly. That’s why we always recommend that our patients visit us every six months for a checkup and thorough cleaning to remove any tartar that may have formed since their last appointment.
If it’s been longer than six months since your last dental appointment, we welcome you to call and schedule a checkup today. We can’t wait to see you!
Re-posted with the permission of Perio Protect.
 One of the strongest defenses we have against virus’, such as COVD-19, is a robust immune system so we can fight infection – that’s why we’re doing our best to help our patients boost their immunity.
One of the strongest defenses we have against virus’, such as COVD-19, is a robust immune system so we can fight infection – that’s why we’re doing our best to help our patients boost their immunity.
There are a number of scientifically-based recommendations to help boost your immune system such as eating nutritious foods and balancing our diet, making sure to get adequate sleep and physical activity, getting outdoors for some sunshine, and managing stress.

But also, research suggests that treating chronic infections, including in the mouth, may help improve immunity.

Poor oral health influences immunity and if periodontal disease (gum disease) is left untreated, it may negatively impact your overall immunity.
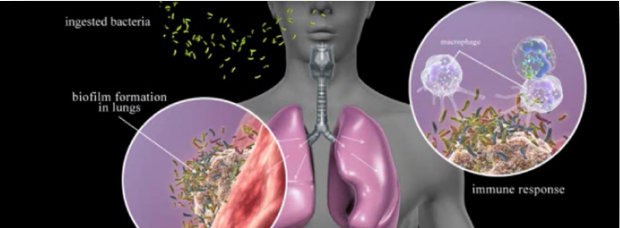
For many years we’ve known that bacteria from gum disease can be aspirated into the lungs. When this happens, the lung’s ability to fight infection is disrupted, which may increase the risk for co-infections, such as virus’, like COVID-19.
That’s why, more than ever before, we’re being especially diligent in examining patients for gum disease or any signs of oral inflammation. And, for those who have gum disease, it’s important to get treated as soon as possible.
Thorough oral hygiene will reduce the bad bacteria in your mouth. That’s a good thing! This includes brushing your teeth twice a day with an anti-microbial toothpaste, and cleaning in between your teeth with floss or pics. A water irrigation device and antimicrobial mouthwashes are other tools for keeping your mouth clean. The goal is to decrease the bacterial burden in your mouth.
© 2020 Casey Hein BSDH, RDH, MBA. All Rights Reserved
